Nerve injuries like cervical and lumbar radiculopathy can disrupt daily life with pain, numbness, and mobility challenges. Discover how cutting-edge treatments can address your symptoms and help you regain mobility and comfort.
Written by

Angel Rigueras
Pain Management Specialist
Share
Written by

Angel Rigueras
Pain Management Specialist
Share
Table of content
Related content
Nerve injuries can significantly disrupt daily life, causing pain, numbness, and mobility challenges.
Whether stemming from cervical or lumbar radiculopathy, these conditions often require specialized care to alleviate symptoms and promote healing. Modern advancements in neuroskeletal care have opened new pathways for effective treatment, combining innovation with patient-centered approaches.
University Orthopedic Care leads the way in offering innovative treatments for nerve injuries, providing a patient-first approach with options like Hyperbaric Oxygen Therapy (HBOT) and nerve block injections that help restore function and comfort.
Nerve injuries occur when the pathways connecting the brain, spinal cord, and body are disrupted, leading to symptoms such as pain, numbness, or weakness. These injuries commonly result from trauma, compression, or underlying conditions like diabetes. Two prominent types of nerve injuries are cervical and lumbar radiculopathy. Cervical radiculopathy involves nerve root compression in the neck, causing discomfort or tingling that radiates to the arms, while lumbar radiculopathy affects the lower back, with symptoms extending into the legs.
Common causes of these injuries include herniated discs, where bulging or ruptured discs press on nerves, and bone spurs, which narrow nerve pathways. Spinal stenosis, or the narrowing of the spinal canal, can also lead to nerve irritation. Additionally, repetitive stress or traumatic events, such as accidents, can exacerbate nerve issues. Recognizing the symptoms, ranging from radiating pain and tingling sensations to muscle weakness and diminished reflexes, is crucial for early intervention and treatment.
Research highlights the importance of early diagnosis and intervention in preventing long-term complications. A study in the Journal of Clinical Neurology emphasizes that timely treatment can significantly improve nerve regeneration and functional outcomes, reducing the risk of chronic pain and disability.
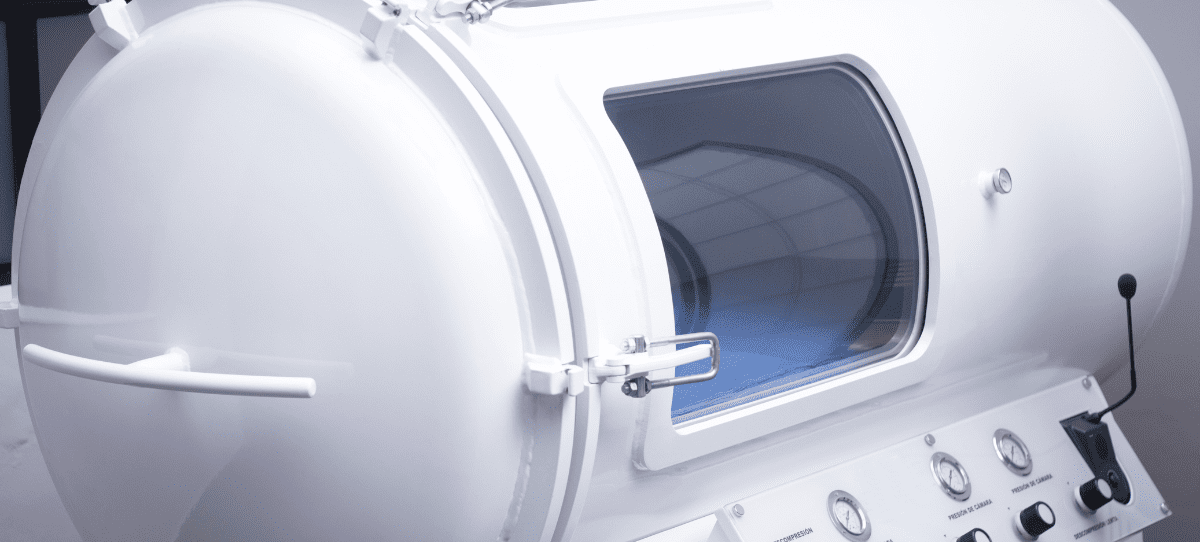
Hyperbaric Oxygen Therapy (HBOT) has transformed the treatment landscape for nerve injuries. By delivering 100% oxygen in a pressurized chamber, HBOT promotes cellular repair and regeneration. Research underscores its effectiveness in reducing inflammation and stimulating angiogenesis, the formation of new blood vessels, which enhances oxygen delivery to damaged tissues. A notable study published in the Journal of Neuroregeneration demonstrated improved motor and sensory functions among patients with lumbar radiculopathy treated with HBOT.
Further research highlights its potential to reduce oxidative stress, mitigate neuronal apoptosis, and accelerate nerve fiber regrowth, showcasing its value as a comprehensive therapeutic option. In traumatic brain injury patients, HBOT has shown the ability to enhance angiogenesis and nerve fiber regeneration, underscoring its broad applicability in neuroregenerative medicine.
Nerve block injections, which deliver anesthetics or anti-inflammatory agents directly to affected nerves, provide precision-targeted pain relief. These injections alleviate acute pain and can aid in diagnosing the root cause of discomfort. Studies reveal their effectiveness in offering immediate symptom relief and facilitating mobility restoration in cases of lumbar radiculopathy and sciatica. Additionally, nerve block therapy serves as an excellent complement to physical rehabilitation, enhancing the effectiveness of comprehensive care plans tailored to patient needs at University Orthopedic Care.
A systematic review in Pain Physician Journal found that selective nerve root blocks are particularly effective in alleviating radicular pain, with patients experiencing significant improvement in functional scores and quality of life. These findings highlight the dual role of nerve blocks as both diagnostic and therapeutic tools.
Physical therapy plays a pivotal role in the healing process for nerve injuries. Tailored programs focus on improving flexibility, reducing nerve tension, and strengthening core muscles to alleviate spinal pressure. Corrective exercises also enhance posture and coordination, helping patients regain mobility and achieve sustainable results. Through these combined efforts, rehabilitation ensures a holistic recovery process that restores quality of life.
Incorporating advanced techniques, such as mild HBOT during rehabilitation, has shown promising results in reducing inflammation and improving nerve oxygenation. Recent studies also suggest that integrating neurofeedback and neuromuscular reeducation into physical therapy regimens can accelerate recovery, particularly in patients with chronic nerve injuries.

Accurate diagnosis forms the backbone of effective treatment. At University Orthopedic Care, advanced tools like Magnetic Resonance Imaging (MRI) and Electromyography (EMG) are employed to evaluate nerve function and pinpoint damage. These diagnostic methods guide targeted interventions, ensuring treatments are precisely tailored to each patient’s condition, enabling better outcomes and minimizing recovery time.
Emerging diagnostic modalities, such as functional imaging and advanced neuroconduction tests, further enhance precision in identifying and addressing nerve damage. A study in the Journal of Advanced Neurology demonstrated that combining traditional diagnostic tools with advanced imaging techniques improved diagnostic accuracy by 25%, leading to more effective treatment planning.
While not all nerve injuries are avoidable, proactive steps can significantly reduce risk. Maintaining a healthy weight alleviates unnecessary stress on the spine and nerves, while regular exercise strengthens core muscles, enhancing spinal support and stability. Simple exercises like planks and bridges are particularly effective. Attention to posture during daily activities, such as sitting or lifting, can prevent strain on the lower back. Ergonomic adjustments in workspaces, including supportive chairs and optimal desk setups, also play a critical role in maintaining spinal health and preventing nerve-related issues over time.
Additionally, adopting a balanced diet rich in anti-inflammatory foods can promote overall nerve health. Foods such as fatty fish, nuts, and leafy greens contain essential nutrients that support nerve repair and reduce inflammation. Engaging in mindfulness practices like yoga or tai chi can further enhance physical and mental resilience, minimizing the risk of nerve-related injuries.
At University Orthopedic Care, our primary goal is addressing and alleviating your pain with advanced, patient-focused treatments. From HBOT to nerve block injections, we combine innovation with compassionate care to deliver solutions that meet your unique challenges. Our expert team ensures every step of your recovery is personalized, prioritizing your comfort and long-term well-being.
Recovering from nerve injuries requires a thoughtful blend of cutting-edge therapies and patient-focused care. Our team of orthopedic specialists utilizes innovative solutions like Hyperbaric Oxygen Therapy and nerve block injections to deliver comprehensive, personalized treatment. Paired with advanced diagnostics and tailored rehabilitation programs, our approach ensures each patient receives the best possible care.
Contact University Orthopedic Care at (866) 962-1744 to learn more about our specialized services. Let us help you restore mobility, reduce pain, and regain control over your life.
Related content
